| TBD Panels | 3-Panel STD Test | 9-Panel STD Test | 5-Panel STD Test | 3 Site: Oral, Rectal, Genital |
|---|---|---|---|---|
| Chlamydia |  |  |  |  |
| Gonorrhea |  |  |  |  |
| Trichomoniasis |  |  |  |  |
| HIV (Ag/Ab) |  |  | ||
| Syphilis |  |  | ||
| Hepatitis B & C |  | |||
| Mycoplasma Genitalium |  | |||
| Herpes I / II |  |

- 8 E Charleston Blvd
- Las Vegas, NV 89104
- Mon - Fri
- 10 AM – 4 PM
- Contact us:
- 702-909-0554
- hello@tbd.health

PAY IT FORWARD
Feel good by contributing – help others to gain clarity on their sexual health. Note: TBD Health Inc. is not a non-profit.
| TBD Panels | 3-Panel STD Test | 9-Panel STD Test | 5-Panel STD Test | 3 Site: Oral, Rectal, Genital |
|---|---|---|---|---|
| Chlamydia |  |  |  |  |
| Gonorrhea |  |  |  |  |
| Trichomoniasis |  |  |  |  |
| HIV (Ag/Ab) |  |  | ||
| Syphilis |  |  | ||
| Hepatitis B & C |  | |||
| Mycoplasma Genitalium |  | |||
| Herpes I / II |  |

By Adrienne Ton, Nurse Practitioner
Q: I’m worried about HPV! I keep hearing people talk about HPV, but I got the vaccine when I was a kid. Can I still get HPV? Should I get screened for HPV? How do I get screened?
A: We have multiple questions here. So TL:DR → Yes, you can still get HPV if you’ve been vaccinated If you’re a person with a vagina and cervix, you should get screened for HPV You can get screened with a test (usually a type of swab) during a cervical cancer screening.
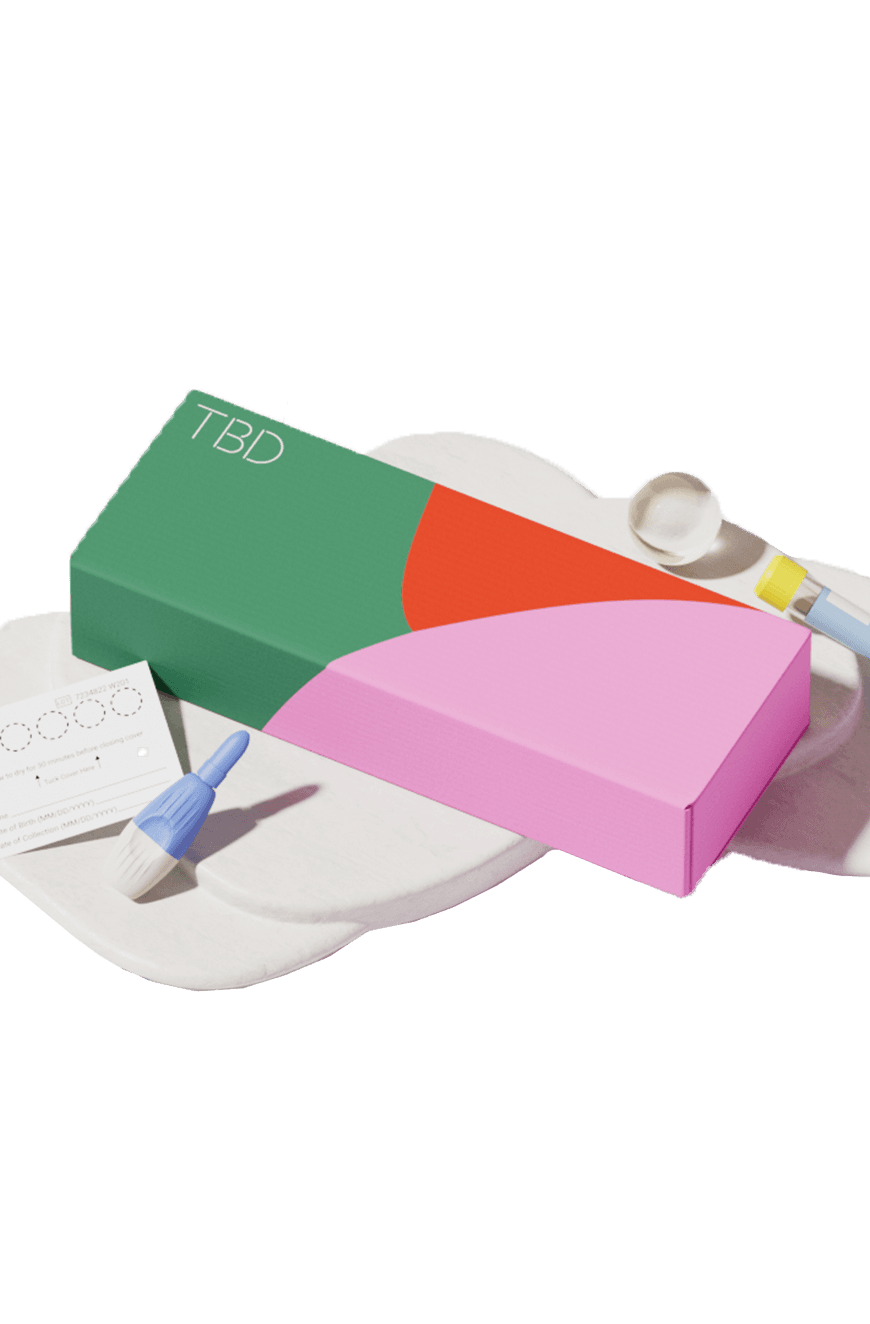
TBD Recommends: Bacterial Vaginosis At-Home Testing Kit
Yes, you can still get HPV if you’ve been vaccinated.
The HPV vaccine is excellent but it does not protect against every type of HPV. The most recent HPV vaccine protects you against 9 of the high-risk strains, but there are over 200 strains of HPV identified so far, many of which are not all high-risk. The vaccine helps protect you against the highest risk strains which are responsible for most cervical cancers and genital warts.
Generally speaking, the Human Papilloma Virus (HPV) is the most common STD (aka STI) so you will likely encounter it if you’re sexually active. If you’ve had sex before, you’ve probably been exposed to the Human Papilloma Virus (HPV). Most people will encounter HPV in their lifetime. I’ve even heard HPV referred to as the “common cold of the STD world”. Most of the time, as in 9 out of 10 times(!), your body will clear the infection up on its own and the infection does not lead to cancer. Rarely, an HPV infection will stick around and sometimes can lead to diseases such as cervical cancers, mouth and throat cancers, anal cancers, and/or genital warts. (For more info on HPV itself, check out our blog about HPV)!
If you’re a person with a vagina and cervix, you should get screened for HPV.
First of all, it’s important to understand what we mean by “screening”. Screening is a test that’s done to look for a disease before it occurs or early in the disease process before significant symptoms occur. Screening tests are usually reserved for groups who have a higher risk for a disease. This can be a different term from “diagnostic testing” which is meant to investigate a cause of an illness (for example: if you have a new rash at your genital area, you might receive diagnostic testing to find out the cause).
Right now, based on the types of tests that are available and current research about the rates of disease like cancer caused by HPV, routine screening for HPV is only recommended for people with a cervix or uterus. Screening is recommended because we have found that this can lead to finding diseases like cervical cancer earlier - before they spread or before they cause symptoms. Finding disease earlier can mean more treatment options and a better chance of success for those treatments.
Learn More: Understanding HPV in Females
In some cases, such as people with cancers like of the mouth and throat or anus, people who don’t have a cervix may get diagnostically tested for HPV.
You can get screened with a test (usually a type of swab) during a cervical cancer screening.
Again, HPV screening is really only currently recommended for people with uteruses as a part of cervical cancer screening, commonly referred to as a pap smear or papanicolou test.
A pap smear, also known as papanicolou test typically checks for abnormal cervical cells that can signify cancer or precancerous lesions. This is done during an in-office exam, in which a healthcare provider uses a small swab or brush to gently collect cells of the cervix and sends them for testing (sometimes called cytology only tests). Depending on the situation, your healthcare provider may also order “co-testing”, which means that they also use that sample to test for signs of high-risk HPV strains that can lead to cervical cancers. This does not involve any difference in how the pap smear is collected, but is just an extra test run with the same sample.
There are a few different large, reputable medical groups who have a difference in recommendations for cervical cancer and HPV screening, which includes differences in when to start screening and when to start HPV testing. Two of the biggest and most trusted groups have slightly different recommendations as follows:
The American Cancer Society (ACS) recommends that people with uteruses wait until the age of 25 to get screened. Between ages of 25-65, they recommend screening with a test that only checks for the presence of high-risk HPV strains every 5 years. They do have some other options for screening, but the HPV-only test is the preferred test.
In contrast, the United States Preventive Services Task Force (USPSTF) recommends earlier screening starting at age 21 and screening more with cytology only (pap smears with lab tests looking for abnormal cells) every 3 years. They do not recommend testing for high-risk HPV infections until age 30. Between age 30-65, there are a few recommended options for cervical cancer screening which include:
- HPV test every 5 years
- HPV/Pap cotest every 5 years
- Pap only test (without HPV testing) every 3 years
Currently, both guidelines are widely used and it may depend on your clinician or organization. But this may change over time with more research and availability of tests. And the screening recommendations will shift depending on what kinds of test results you’ve had in the past.
So what does that mean for you?
If you have a uterus and are wondering about HPV testing, I’d recommend getting scheduled for cervical cancer screening and discussing the options with your healthcare provider. For most people, I often recommend starting to think about cervical cancer screening at least at age 25. This might be different based on the tests you have available in your clinic and/or what kinds of testing frequency you prefer! Getting screened (period!) with either guideline if the testing is available is a good option.
I’d also recommend that you keep track somewhere (maybe the notes app on your phone or a file with your general medical records) of your cervical cancer screening results and dates if you have those available. Those will be helpful in determining monitoring of abnormal test results (if they occur).
FYI: You can also get tested for HPV only, like through TBD’s home test kit. This helps you identify the presence of HPV - which is the leading cause of cervical cancer! It’s important to note that this is not exactly the same as a routine cervical cancer screening like you would do in-person. The difference is that during an in-person exam, a clinician would typically collect the sample of cells and/or fluid from the cervix, but the home-test uses a sample from the vagina. However, there are more research studies showing promising aspects of self-collected HPV tests so it’s possible that home HPV testing may be a part of routine cervical cancer screening in the future.
---Adrienne, Nurse Practitioner
This article provides information about sexual health, healthcare and/or related subjects. The blog content and any linked materials herein are not intended to be, and should not be construed as a substitute for, medical or healthcare advice, diagnosis or treatment. Any reader or person with a medical concern should consult with an appropriately-licensed physician or other healthcare provider. This blog is provided purely for informational purposes. The views expressed herein are not sponsored by and do not represent the opinions of TBD Health Inc.
Email us and a team member will get back to you within 24 hours. We’re also available via call or text at +1 (702) 909-0554
Sign up below to get 10% off
By providing my email address, I agree to receive email with marketing communications from TBD Health including news, promotions and exclusive offers. I understand that I can opt out at any time by using unsubscribe links. Visit our Terms of Service or Privacy Policy for more information.